The Knee Joint
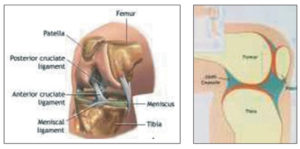
The knee joint is one of the most complex joints in the body. Apart from bending and straightening; it allows other complex movements such as rotation and gliding. The natural knee consists of three bones: the thigh bone (Femur), the shin bone (Tibia) and the knee cap (Patella). The lower end of the femur, the upper end of the tibia and the undersurface of the patella are all covered by articular cartilage. The articular cartilage is a tough and a very smooth material that ensure smooth and pain free movement of the knee. Between the two ends of the femur and tibia lies cartilaginous tissue known as Meniscus, which acts as padding. The knee joint is enclosed in a joint Capsule. The inner surface of the joint capsule is lined with the synovial membrane that produces synovial fluid (a viscous fluid that provides friction free movement). Working together, the synovial fluid and menisci, act as a shock absorber. They absorb the powerful forces the impact on the joint during exercise and activity. Envelopes of tough ligaments connect the femur and tibia, covering the joint and stabilizing it. The knee’s movements are initiated and controlled by the strong muscles of the thigh and lower leg. A healthy knee joint will allow the leg move freely within its range of motion, while absorbing the impact that results from activities such as walking and running.
About Knee Joint Replacement
The aim of knee replacement surgery is to:
- Relieve your pain
- Correct any deformity for example, bow leg or knock knee
- Restore any loss of function to your knee
- Improve your quality of life
Knee joint replacement surgery involves resurfacing the ends of the femur, the tibia and if necessary the underside of the patella with man made components, called prostheses. It is a resurfacing operation and not the Replacement operation, which is actually a misnomer. Knee prostheses are designed to simulate the human anatomy as closely as possible and present day prostheses are very well researched and safe. There is no allergy ever reported in any of the joint implant. There are many different designs of knee prosthesis available and your surgeon will choose the one considered most suitable for you. However, the final decision may need to be made at the time of your operation.

Components of A Knee Replacement
Each knee prostheses are made up of several parts.
1. The femoral component resurfaces the femur. The femoral component is made of a metal alloy.
2. Although the patella is not always resurfaced, the patella component resurfaces the undersurface of the patella that rubs against the femur. The patella component is either made completely of plastic or plastic with a metal alloy back.
3. The tibia component can be a single or two piece design. The single piece is made of plastic. While the two pieces design consists of metal tray that is secured to the bone and a plastic insert that provides a smooth surface on which the femur moves. The plastic insert may be attached firmly to the tibia tray or may be designed to move relative to the tibia tray (mobile bearing designs)

The Operation
The operation usually takes 1-1.5 hours depending on the severity of the disease in your knee.
Step1
After making the incision (cut) in the skin, the knee joint is exposed
Step 2
The damaged surfaces of the femur and tibia are then removed and the underlying bone is prepared to accept the prosthetic components under computer guidance
Step 3
Once your femur and tibia are prepared, the femoral and tibia components are fixed to the bone with the help of bone cement
Step4
During the surgery, we will have the chance to take a closer look at your patella. If we decide to resurface your patella, the damaged surface of patella is removed and prepared to accept the prosthesis. The patella prosthesis is then fixed to the undersurface of the patella with the help of bone cement
Step 5
During the procedure we will ensure that the movement in your knee are full, smooth and stable.
At Home
To manage your daily activities after your knee replacement. Upon returning home you will need help for the first few weeks. You will need to continue taking your regular medications and continue exercising as directed by your physiotherapist and surgeon. Remaining active and practicing the prescribed exercises are the quickest ways to full recovery, you have every reasons to expect to regain the full use of your leg. However this will take time.
Preparing Yourself For Surgery
Commit to the success of your surgery, working as a team, you and your family should adopt a positive attitude towards the success of your surgery.
Remain as active as possible. Remaining active while waiting for your surgery is an important key to the success of your surgery. Studies have shown that the stringer and more flexible you are before your operation the quicker you will recover and more flexible you will be after your operation. Gentle exercise such as walking, range of motion exercise and swimming can be very beneficiary.
DIET
Diet is especially important in times of stress such as surgery. Be sure to include as many iron rich foods in your diet as much as possible. For example beans, nuts, dried fruits and meat if you are taking non vegetarian diet.
Stop smoking. If you have not already done so, it is suggested that you stop smoking. This will help reduce the risk of complications during and after your surgery. If you would like some advice and support please let us know and we will try to help.
Make sure all infections are cleared up prior to surgery. These include; tooth abscesses, bladder infections, infected leg ulcers, cold and the flu. You must notify me as soon as possible if you are suspected of or diagnosed with an infection, as we may have to reschedule your surgery.
Stop Taking Medications
If you have any questions as to whether you should continue to take certain medications,please ask my assisting staff.
Skin
It is important that your skin does not have any open sores or wounds (such as infected corns, bunions, insect bites) and is free from infection before your operation. This is especially important if you have problems such as eczema or psoriasis. If problems such as leg ulcers or skin rashes develop you should see your local doctor.
Existing Medical Condition
It is important that existing medical conditions are kept in check such as diabetes and that any problems which may develop are dealt with quickly, as they may lead to your operation being postponed. One of the most common problems requiring treatment prior to surgery is high blood pressure (hypertension). If you know you have this condition it may be helpful to have your blood pressure checked.
What To Bring To Hospital
Please see the following checklist
- Non-slip, non-lace and flat closed in shoes if possible
- Comfortable clothing that is knee length including a mid length robe Current walking device (if using any)
- Toiletries X-rays
- All medications you take regularly Books or magazines to read
- Radio and headphones Hearing devices
- Dentures and containers (if applicable)
- Please do not bring any valuables to hospital with you Please leave all your jewellary at home or with relatives
Pre-Screening & Laboratory Tests
Before having your surgery, several laboratory and pre-screening test must be completed. These will be done either before or during your admission. This will help us in assessing your health prior to surgery.
At The Hospital The Anaesthesia
The type of anesthesia you have will depend upon you and the anaesthetist. You may opt between a spinal, epidural form of anesthesia or general anaesthesia. The surgery usually takes 1-2 hours to complete.
Recovery Room
When the operation is completed, our team will contact your family or friends to update them on the success of your surgery. You will then be taken to the recovery room. A nurse will be with you to monitor your vital signs. If you have pain, medication will be provided. Usually in my cases after surgery pain is negligible. You will be encouraged by nurses to take deep breath and cough to help clear lungs. When you are fully conscious and stable you will be taken back to your room/ward.
In Your Hospital Room After Surgery
When you return to your room from recovery you will continue to be monitored by the nurses. Patients are made to stand 2 hours after surgery. This gives a lot of confidence to the patient and helps in further recovery and physiotherapy. On the first day after surgery, you may begin drinking fluids and eating meals. The intracath line will remain in your arm for one or two days to administer fluids and antibiotics. This helps prevent infection and gives you proper nourishment until you are eating and drinking comfortably. We will ensure that you have a painless recovery. A specialized unit of pain management team will be looking after you. But still you can feel some pain and discomfort after surgery. Be sure to inform your nurse of your pain so that the dose of medication will be adjusted. You will be made to walk inside the room, the next day after surgery and outside the room on 2nd day. Your toilet training will start 2nd day of surgery. Me & my team will visit you to discuss your surgery and progress. Blood samples may also be taken to check your condition. Regular medication is given to maintain your level of comfort and allow you to participate in physiotherapy.
Wound Care
Your wound must stay clean and dry until it fully heals
Starting Your Physiotherapy
Physiotherapy visits starts soon after your surgery. Patients are made to stand 2 hours after surgery. The patients will stand and walk inside the room on first day of surgery and outside the room on 2nd day of surgery. The physiotherapist will continue to see you on a daily basis to progress your rehabilitation program in consultation with us. You are encouraged to commence the knee range of movement and strengthening exercise program as soon as you get back from recovery. The exercise described on the following pages should only be done on the advice of your physiotherapist. Your first task will be to learn how to get out of bed, sit and stand safely with your physiotherapist assisting you. You will start to walk using a frame or a pair of crutches. This is usually practiced 2-3 times a day under supervision. As you progress and your confidence builds, you will be able to walk on your own with the use of a walking aid.
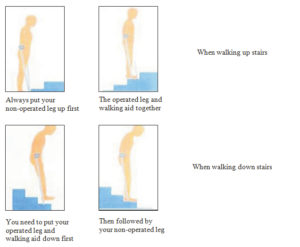
Your physiotherapist will progress you onto practicing walking up and down stairs. At the same time, your physiotherapist will be graduating your knee exercise program accordingly. The objective of these exercises is to train and strengthen your muscle so that you benefit fully from your operation.
Most patients immediately benefit from surgery. The first few months after surgery involve a commitment, motivation and work on your part to get the knee working properly. The objective of your physiotherapist is to help you benefit fully from your operation. The more actively you participate, the quicker your recovery will be. Your rehabilitation program is designed to meet your personal needs.
Your physiotherapist will give you an exercise program. This will help strengthen the muscles and keep joints mobile, reduce the risk of blood clots, prevent chest infection and subsequently assist to speed your recovery.
Breathing Exercise
Regular deep breathing and coughing practiced in the seated position will help keep your lungs clear and free from congestion. Take ten deep breaths, holding each breath for 3 seconds, followed by a strong cough each hour. Smokers should stop smoking at least four weeks prior to their surgery so the lungs will be cleared of phlegm, to reduce the risk of chest complications following surgery.
General Guidelines: After Surgery
Exercise after surgery will help you recover and regain the movement and strength of your knee. Exercise also helps to:
- Reduce swelling
- Prevent blood clots
- Control your pain
- Prevent constipation
- Improve your sleep
Check with your physiotherapist for guidance about the best way to warm up your new joint. Your physiotherapist may tell you to:
- Apply moist heat to the front and back of the thigh (NOT your knee) for 5-10 minutes to improve blood flow
- Walk forward, backward or sideways for 5-10 minutes
- Use a stationary bike (upright or seated) for 5-10 minutes

Tips For Using A Bike:
- Raise or lower the seat so your operated leg is almost straight
- Rock the pedals gently back and forth
- When you are ready, do a full circle
- Cycle forwards and backwards
- Slowly add light resistance
- Lower the seat as your knee range of motion improves
TO KEEP PAIN AND SWELLING UNDER CONTROL:
1. Rest Your Joint
- Change positions often (every 20 minutes) when you are awake. Try sitting, standing, and walking.
- Pace yourself. Have a rest day after a busy day.
- Lie down 3 times a day for 30 minutes on your bed or sofa. Put your leg up and support it with a wedge, arm rest of couch, or with pillows (as shown).
- Keep knee straight on the pillows with foot and ankle higher than heart

2. PUMP YOUR ANKLES
- If you are lying down, move feet up and down
- If you are sitting, place feet flat on floor, lift toes up then lift heels up
- Repeat______________times.
- Repeat______________times per day.

3. USE ICE
Ice your knee when it is hot and red, painful and after exercises.
Ice fomentation is a very safe and effective method to reduce pain and swelling around Knee after surgery.
Follow These Steps:
- If your scar is not healed, cover it with a clean bandage and a sheet of clean plastic wrap. Put a flexible gel pack or plastic bag with crushed ice on your knee.
- Ice pack should be applied on the posterior aspect and on the sides of the knee. Avoid the anterior aspect with the scar mark.
- Leave the cold ice pack ON for 10 minutes.
- Take it OFF for 10 minutes.
- Then put it back ON for 10 minutes.
- Repeat every hour for 10-15 minutes.
To help with knee bend, place ice over your knee with your knee as bent as possible.
To help with knee straightening, place ice over your knee with your knee as straight as possible.
4. Use Pain Medicine
Use your pain pills as prescribed by your doctor or surgeon. Tell your doctor or surgeon if the pain is too much or not improving.

5. Use Walking Aids
Use the walking aid that your physiotherapist has measured and recommended. Do not change or stop using the walking aid until your physiotherapist or surgeon tells you to. Walkers, crutches and canes help to:
- Reduce the stress on your knee
- Reduce pain
- Improve your walking
- Improve your balance and reduce falls
Tips For Walking:
- Start by walking on a flat, even surface
- Wear supportive non-slip shoes
- Bend your knee with each step
6. SLEEP
Sleep helps with rest and recovery. It is normal to have some sleepless nights up to 12 weeks after your knee surgery.
Tips For A Better Sleep:
- Ice your knee before bed to help with pain
- Do gentle knee movements and ankle pumps to help relax the muscles around your knee
- When sleeping on your side, put a pillow between your knees
- When sleeping on your back or on a reclining chair, use pillows to support your leg and keep your knee straight
Strength & Motion Exercise
Ankle range of Motion Exercises Repeat…..times X…..a day
STATIC QUADRICEPS
Repeat…..times X…..a day

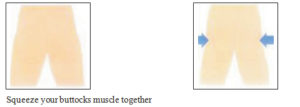
STATIC GLUTEALS
Repeat…..times X…..a day
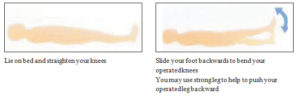
KNEE RANGE OF MOTION
Repeat…..times X…..a day

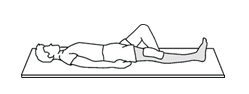
STRAIGHT LEG RAISES
Repeat…..times X…..a day
INNER RANGE QUADRICEPS
Repeat…..times X…..a day
KNEE FLEXION
Repeat…..times X…..a day

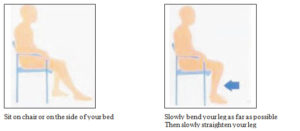
KNEE EXTENSION
Repeat…..times X…..a day
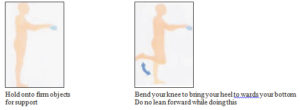
STANDING KNEE FLEXION
Repeat…..times X…..a day
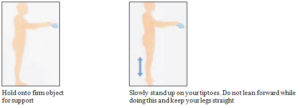
STANDING HEEL RAISES
Repeat…..times X…..a day
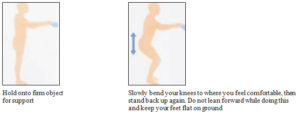
Available Walking Aids
Repeat…..times X…..a day
AVAILABLE WALKING AIDS
There is a variety of different walking aids available from which your physiotherapist could choose from for you to use after your operation.
As you recover and become stronger, requiring less support, your physiotherapist will appropriately change the walking aid you use.
Below is a list of possible walking aids that you may use.

How To Use The Stairs
Home Programme:
Home programme will be easy and painless if you painless if you co-operate. This has been summarized as below:
Supine Position (Lying On Back)
- For flexion deformity, keep two cushions under the heel and press the knee down (think a water bag is placed under the knee) feel the contraction, 5 repetitions by self (active) count loud upto 10 then Relax.
- Support person will passively push the knee down for stretching and ask the patient to relax, holding the knee pressed till patient feels mild discomfort. Count upto 10 (5 repetitions).
- Heel slides actively by self and active assisted, when maximum flexion is achieved apply a little pressure to increase range towards flexion.
- SLR Theraband assisted Straight leg raise. Keeping the knee tight and then raise the hip not too much pressure on the theraband. Count upto 10 then relax (5-10 repetitions).
Side Lying Position
- Knee bending on your own as much as possible, then count upto 10 then straighten (10 repetitions).
- At maximum flexion (bent position). Doctor will push a little further ending to level of discomfort but no pain. Hold for a count of 0-10 (10 repetitions).
- End arc quadriceps contraction against resistance Vs flexion 5:1
In Standing
- Gait training (walking)
- Keep the knees exposed: Small steps, bend the knees, equal weight on both feet, Heel strike
- Tip Toeing (standing on toes with minimal support) 10 repetitions + count till 10.
Sitting Position (High Chair)
- Active (by self) bend the knee as much as possible. Hold & count of 10 (10 repetitions).
- The support person will push into further flexion (towards bending) after maximum range is achieved at the same time ask patient to hold hands and tighten/take deep breaths.
- Keep a chair in front to support the heel and press the knee down hold and press the knee down hold for count of 10 (10 repetitions).
- The support person will press the knee down. Patient to press by self to relax knee dangling (free swinging) 10-20 reps.
- Keep back well supported at all times. Repeat these exercise by self as many times as comfortable.
Way To Conserve Energy
Sit-Don’t’ Stand
Sit instead of standing during daily activities such as, brushing your teeth, getting dressed, showering etc. in the first four weeks of the surgery.
Sitting Position (High Chair)
- You need sleep after major surgery
- Take a nap in the afternoon
- Take five-ten minute break during activities
- When resting, change your position every 20 minutes to avoid stiffness
Reduce The Effort Required To Do Daily Activities By:
- Planning plan daily schedule of things to do. Set priorities, alternate heavy and light duties, and allow for frequent breaks.
- Positioning-use proper working heights whenever possible. Eliminate any unnecessary bending, reaching, and stretching.
- Protection protect your joints from excessive strain. Change positions frequently
ON GOING RECOVERY
Driving
- You should not drive until otherwise advised. This may be 4-6 weeks after your surgery. The reason for this is that your personal safety is the main concern. You need good control and coordination of your leg to work the accelerator and brake.
Returning To Work
- This may be 2-6 weeks after your surgery. It will depend on the type of work you go back to. The reason for this is that your personal safety is the main concern and everyone recovers at different rates.
Diet
- There are no restrictions to your diet. But bear in mind that you have just undergone major surgery, so make sure you eat plenty of fruits and vegetables and pulses, beans and lean meats for protein and iron. Try and drink 6-8 glasses of water a day.
Sport And Activities
- Your new prosthesis is designed for activities of daily living, not high impact sports. You may involve yourself into light sports activities for sure. Walking, swimming and cycling are recommended. Aggressive sports, such as running, jumping, repeated climbing and heavy lifting may impair or compromise the function and long term success of your joint and therefore should be avoided.
Metal Detectors
- Your new prosthesis contains metal which may be noted by metal detectors and security devices.
- For this reason, you will be given a card that verifies that you have had a joint replacement and have received a metal prosthesis. Your orthopaedic surgeon’s name and telephone number will be on the card.
How Long Will My Knee Replacement Last
In ideal circumstances a new knee joint would function well and last you for the rest of your life, especially if it is a mobile bearing joint. How long your knee replacement will last depends on many factors such as:
- Your physical condition
- Your weight
- How active you are
- Type of joint (implant) used for you
- Stability of your new knee.
Short & Long Terms Care Ofyour New Knee
You can protect your new knee by taking a few simple steps
Watch For And Prevent Infection. Here Are Some Of The Warning Signs You Must Look Out For:
Increasing pain or swelling in the calf
Wound becoming red or oozing
Pain that is not relieved by medication
You MUST contact us immediately if the above symptoms occur. If you get an infection anywhere in your body (for example: skin, urine, chest, throat, teeth) the infection can get into the blood stream and spread to your knee. Please notify me or my team if you are being placed on a course of antibiotics.
Follow Up Care
When you leave the hospital, you will be given a schedule of follow up visits. These visits will ensure the long-term success of your operation. We want to check you several times in the first year and annually after that. Often, x-rays are taken prior to each follow up to confirm the well being of the prosthesis.
Weight Control
Keeping your weight under control is preferable. It will reduce the amount of pressure and stress on your new knee. You will be able to reduce weight more easily after surgery as now your activity will be unlimited.
Surgical Procedures
If you are scheduled to have surgery in the future, even minor surgery, such as a mole removal, ingrown toenails, eye surgery, or any dental work, you must notify me or my team. This also applies to any invasive procedure using a special scope, such a cystoscopy, or gastroscopy. The reason for this precaution, is that we may want to put you on antibiotics as a precautionary measure to make sure that you do not develop any infection that may cause harm to your new joint.
FACTS ABOUT HEALTHY BONES, OSTEOPOROSIS AND GRACEFUL AGING

India: Hard Facts
- Over 36 Million Indians have osteoporosis.
- 80% of them are women.
- On a global basis, Indians have the highest prevalence of osteopenia.
- Osteoporotic fractures are more common in Indian men than in the West
What Makes Us More Prone?
- Indians have a poor calcium and protein intake in diet
- Vitamin- D deficiency is common due to poor exposure of skin to sunlight.
- Excess salt intake – may increase urinary loss of calcium\
- Healthy exercise is neglected
- Significantly lower BMD
- Awareness about Vitamin D deficiency and general bone health is low

Osteoporosis Leads To Weak Bones.
Weak bones in elderly leads to pain in joints and bones especially the lower back. This pain can be debilitating and can further leads to loss of independence of the patient. Patient may become dependent on others for day to day activity of life. In elderly this osteoporosis can lead to compression fractures of the spine and leads to increased curvature of the spine and ultimately restricted mobility. In case of fall, these patients can have fractures around the hip, wrist or spine, which may require hospitalization and surgical interventions. Epidemiology: India
- Among those who live to 90 years old, 1/3 of women and 1/6 of men will have sustained osteoporotic fracture
- Hip fracture mortality at 1 year is approaching 24%

Non-Pharmacological Treatment
- Calcium & Vitamin-D
- Prevent Fall
- Exercise
- Dietary intervention
CALCIUM & VITAMIN-D ARE USEFUL FOR US AS:
Calcium
- Provides structural integrity of skeleton
- Calcium plays a role in muscular, neural and most metabolic processes
- Everybody needs adequate calcium intake, but especially those at risk for osteoporotic fractures
VITAMIN D
- Bone mineralisation
- Calcium absorption from small intestine
- Extracellular calcium homeostasis
- Deficiency predicts falls in elderly women in nursing homes
CALCIUM IS REQUIRED ON A DAILY BASIS
- 99% of calcium is located in the skeleton Recommended calcium intake
| Adult men and women Women over 50 yrs Men over 70 yrs Pregnant women Lactating women |
1000 mg 1300 mg* 1300 mg* 1100 mg 1200 mg |
Who Needs More Calcium?
- Old age
- Social disadvantage
- Malabsorption due to gastrointestinal disease
- Corticosteroid use
- Sex hormone deficiency
BEST SOURCE OF VITAMIN D : Sun exposure
According to Health Canada the recommended dietary allowances (RDA) for vitamin D are:
| AGE GROUP | RDA | TOLERABLE UPPER INTAKE |
| Infants 0–6 months Infants 7–12 months Children 1–3 years Children 4–8 years Children and Adults 9–70 years Adults > 70 years Pregnancy & Lactation |
400 IU* 400 IU* 600 IU 600 IU 600 IU 800 IU 600 IU |
1000 IU 1500 IU 2500 IU 3000 IU 4000 IU 4000 IU 4000 IU |
Note*: Adequate Intake rather than Recommended Dietary Allowance